Introduction: Acute GVHD (aGVHD) contributes to poor outcomes and increased healthcare resource utilization (HRU) after allogeneic stem cell transplantation (allo-HCT). However, HRU and the economic burden of aGVHD based on severity of the disease and organ involvement is not well characterized. We examined the HRU, cost and mortality associated with aGVHD severity from initial hospitalization (index admission) up to 100 days post allo-HCT.
Methods: Study cohort included 290 adult (≥ age 18) recipients of a first allo-HCT at the University of Florida between 1/2010 and 1/2019. The electronic medical records were reviewed for all patients who developed aGVHD as well as 116 patients without aGVHD who lived at least 1 month after HCT. Clinical measures that characterize the severity of aGVHD and extent of organ involvement were collected from electronic medical records. Medical costs and total hospital days were retrieved from administrative data that allocate costs to services based on departmental input for resource use and were adjusted to 2018 dollars. Wilcoxon rank sum test was used to compare number of inpatient days and total cost. Chi-squared test was used to compare ICU admission rate. Multivariable linear regression was fitted on log transformed cost. Results are shown as cost multipliers that represent ratios on original cost scale.
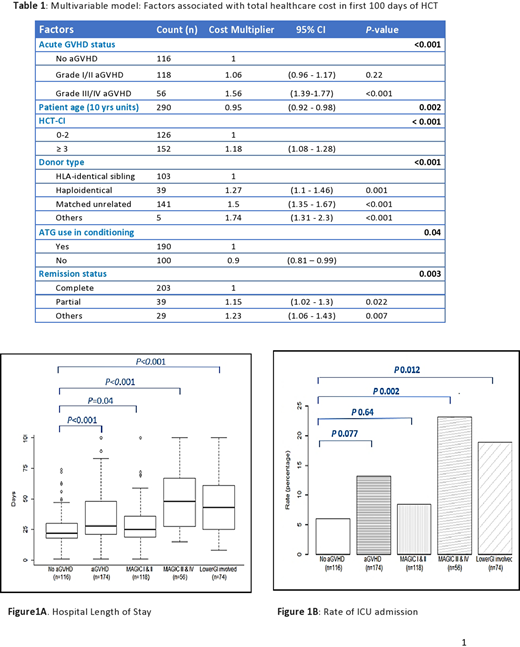
Results: Of the 290 patients, 174 developed aGVHD within 100 days of allo-HCT. A higher proportion of patients with aGVHD had a Karnofsky performance status <80%, underwent matched unrelated donor HCT, and received calcineurin based GVHD prophylaxis. The mean number of days in the hospital for patients with aGVHD compared to those without aGVHD was 28 vs. 22 days, P<0.001 (Figure 1A). The mean number of hospital days for patients with grade I-II compared to those without aGVHD was 25 days vs. 22 days (P= 0.04) and for grade III-IV the mean number of days in the hospital compared to those without aGVHD was 48 days vs. 22 days (p < 0.001). In addition, presence of Lower gastrointestinal (GI) aGVHD was associated with more mean number of days in the hospital compared with those without aGVHD (43 vs. 22 days, P< 0.001). The ICU admission rates in patients with and without aGVHD were 13.2% and 6%, respectively (P=0.07) (Figure 1B). Analysis of ICU admissions based on grade of aGVHD revealed a significantly higher rate of ICU admission among patients with higher grade (grade III-IV) acute GVHD compared to those without aGVHD (22.3% vs. 6.0%, P=0.002). The early mortality rate in the first 100 days in aGVHD patients was twice that of the no aGVHD patients (14.9% vs. 7.8%; P=0.09). Compared to patients without aGVHD, early mortality was significantly higher in patients with aGVHD grade III-IV (7.8% vs. 33.9%; P< 0.001) and lower GI aGVHD (7.8% vs. 25.7%; P=0.001).
Development of aGVHD was associated with a significantly higher total (inpatient and outpatient) cost. The mean total cost for patients with and without aGVHD were $226,545 and $165,622, respectively (P<0.001). Mean total costs associated with grades I, II and III-IV aGVHD were $183,693 (p = 0.44), $201,737 (p = 0.04) and $286,551 (<0.001), respectively (compared to $165,622 for those without aGVHD). Acute GVHD with GI involvement was significantly associated with higher mean total cost compared with aGVHD without GI involvement ($255,283 vs. $177,151, P<0.001). Among aGVHD cohort with GI involvement (Lower and/or upper GI), the mean cost was higher in patients with lower GI (LGI) compared with those without LGI aGVHD ($280,290 vs. $203,879, P=0.04). A multivariable analysis of risk factors for HCT cost identified presence of aGVHD, younger age at HCT, higher comorbidity index, and donor other than matched related donor as being associated with significantly higher costs (Table 1).
Conclusion: HRU, cost, and clinical outcomes were associated with the severity of aGVHD. Development of higher grades of aGVHD and LGI aGVHD were associated with a poor clinical outcome and considerably increased healthcare economic burden. Given these clinical and economic risks it is imperative that new therapeutic strategies are developed for this patient population.
Farhadfar:Incyte pharmaceutical: Other: Member of GVHD advisory forum; CSL Behring: Research Funding. Leather:CSL Behring: Research Funding. Itzler:CSL Behring: Current Employment, Current equity holder in private company. Wingard:CSL Behring: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal